The retina is a very thin and delicate tissue. Traction can be exerted upon it by the vitreous, the clear gel that occupies the back compartment of the eye where the retina is located. In doing so, a retinal tear may develop. Most often, this occurs through normal aging of the vitreous although sometimes trauma to the head or eye may also do this (for more information please read the section on posterior vitreous detachment). Retinal tears are more likely to develop in individuals who are highly myopic (near sighted) and thus generally have a longer eyeball which subjects the retina to more stress from the vitreous.
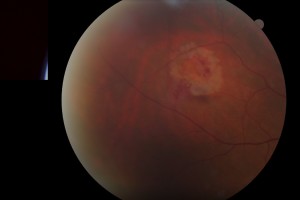
Photo of retinal tear
When the retina is torn, patients may experience the onset of flashes of light due to pulling of the vitreous on the retina as well as new floaters above and beyond what they typically experience. It is important to know that the symptoms of a vitreous detachment, retinal tear, or early retinal detachment are very similar.
A retinal tear is usually treated in the office with a laser procedure to create a barrier of scarring in hopes of preventing a retinal detachment. You can imagine this as spot welding around the tear to create a seal to the underlying tissue.
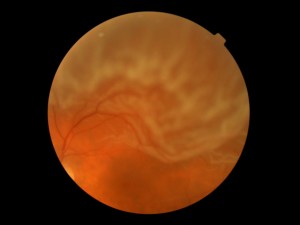
Photo of retinal detachment
A retinal detachment typically occurs when liquefied vitreous over time enters through a retinal tear, thereby separating the retina from the wall of the eye. As previously mentioned, detachments occur usually in the setting of a posterior vitreous detachment and sometimes with trauma to the head or eye. As a result, an area of blurry vision corresponding to the location of the detached retina may develop, especially if the detachment encroaches upon the central portions of the retina. Over time more of the retina will detach, causing further loss of vision.
Depending on the severity and nature of the detachment, there are different treatment options including laser, pneumatic retinopexy, vitrectomy, and scleral buckling.